WHAT: Meet and greet with Jeff Richardson, the newly appointed CEO of Integral Care. This is a unique opportunity to interact with Mr. Richardson and learn about his vision for Integral Care. There will also be an opportunity for B-roll of the Central Texas African American Family Support Conference.
WHO: Jeff Richardson, Incoming CEO, Integral Care
WHEN: Tuesday, February 6, 11:30 AM – Noon
WHERE: Palmer Event Center, 900 Barton Springs Road. Parking available on round about off Riverside Drive.
We invite all media representatives to join us at this event. Jeff Richardson looks forward to meeting you and answering any questions you may have about his new role and the future of Integral Care.
About Integral Care:
Integral Care improves the lives of adults and children living with mental illness, substance use disorder and intellectual and developmental disabilities in Travis County. Our services include a 24-hour helpline for anyone who needs immediate support, ongoing counseling to improve mental health, drug and alcohol treatment to help with recovery, and housing to regain health and independence. As the Local Mental Health and Intellectual and Developmental Disability Authority, Integral Care has pioneered high-quality, community-based care since 1967, collaborating with partners to build a supportive network and combat mental health stigma in Austin.
To learn more about Integral Care, visit our website at: www.integralcare.org
For media inquiries or further information, please contact:
Dr. Kathleen Casey, Chief Strategy, and Innovation Officer
(512) 445-7771
January 16, 2024
Integral Care Announces New CEO
MEDIA ADVISORY
[For Immediate Release]
Media Contact:
Dr. Kathleen Casey, Chief Strategy, and Innovation Officer
(512) 445-7771
kathleen.casey@integralcare.org
Integral Care Announces New CEO
AUSTIN, Texas (January 16, 2024)
Integral Care is delighted to announce Jeff Richardson as Integral Care’s new Chief Executive Officer. Mr. Richardson is an experienced clinician and outstanding leader who brings vision and passion to our vital mission of ‘healthy living for everyone.’ “Jeff’s appointment embodies our commitment to advancing behavioral health and intellectual and developmental disability services and ensuring compassionate, quality care for all individuals in our community”, shared Board Chair, Patricia “Trish” Young Brown.
 “I am privileged to join Integral Care, an organization with core values and dedication to the well-being of all children, individuals, and families that I share,” said Mr. Richardson. “I look forward to building upon the strong foundation and excellent work of David Evans and his team. I am excited to join such a mission-driven organization.”
“I am privileged to join Integral Care, an organization with core values and dedication to the well-being of all children, individuals, and families that I share,” said Mr. Richardson. “I look forward to building upon the strong foundation and excellent work of David Evans and his team. I am excited to join such a mission-driven organization.”
After a highly impactful 30-year tenure as CEO of Integral Care, David Evans announced his plans to transition out of his role earlier this year. Mr. Richardson’s selection is the result of a rigorous six-month executive search process that involved staff and community stakeholder input along with 3 public forums. In his new role as CEO of Integral Care, Jeff Richardson is committed to supporting a strong workforce and leading the organization to new heights. He aims to strengthen Integral Care’s position as a trusted partner in the community, enhancing access to high-quality behavioral health services and promoting health equity for all residents of Travis County.
About Jeff Richardson:
Jeff Richardson was the Vice President and Chief Operating Officer of Sheppard Pratt, a prominent behavioral health organization in Maryland. Serving over 70,000 people across 380 locations, Jeff demonstrated exceptional leadership in the behavioral health sector. His impressive career includes a twenty-three-year tenure as the Executive Director of Mosaic Community Services, highlighting his dedication to community-based care. Jeff holds a master’s degree in social work from the University of Maryland and a master’s in business administration from Loyola University. His commitment to behavioral health advocacy is evident through his involvement in nonprofit boards and state task forces. Jeff has held prestigious roles such as Board President for The National Council for Behavioral Healthcare and President of the Board for the Mental Health Association of Maryland.
Furthermore, Jeff’s contributions to the field extend to consulting, publications, and presentations on critical behavioral health topics, including systems redesign, business development, community mental health, strategic planning, affordable housing, healthcare technology, clinical services and nonprofit mergers and acquisitions.
Beyond his professional achievements, Jeff is a devoted family person, married with four adult children, one of whom has special needs. This personal experience fuels his passion for providing effective and quality behavioral health services to individuals and families facing similar challenges.
David Evans will continue to serve as CEO until Mr. Richardson’s official start date on March 29. Jeff looks forward to scheduling “meet and greets” across the community in the near future.
The Integral Care team welcomes Jeff Richardson as the new CEO and looks forward to a bright future of innovation and progress in behavioral health.
Integral Care is committed to fostering health and well-being for individuals in Travis County, supporting those facing mental illness, substance use disorder and developmental disabilities. By providing essential services like a 24-hour helpline, ongoing counseling and housing assistance, we empower our community to regain independence. As the Local Mental Health and Intellectual and Developmental Disability Authority, Integral Care has pioneered high-quality, community-based care since 1967, collaborating with partners to build a supportive network and combat mental health stigma in Austin.
December 4, 2023
Integral Care Hosts Community Forums to Meet CEO Finalists
MEDIA ADVISORY
[For Immediate Release]
Media Contact:
Jessica Casarez
Jessica.Casarez@integralcare.org
Integral Care Hosts Community Forums to Meet CEO Finalists
AUSTIN, Texas (Dec. 4, 2023) – After a rigorous national search, Integral Care’s Board of Trustees CEO Search Committee has recommended final candidates. The Local Mental Health and Intellectual and Developmental Disabilities Authority is inviting members of the community to attend three open forums. Each event will feature an introduction to one of the candidates, followed by an opportunity for attendees to submit questions. After each Q&A session, the public will be invited to meet the candidates personally. Details of each forum are outlined below.
Dates:
Candidate 1: Tuesday, December 5
Candidate 2: Wednesday, December 6
Candidate 3: Thursday, December 7
Time:
5:30 – 7:00 p.m. CT
Location:
Rudy Zapata Room, Integral Care’s Dove Springs
5015 S. IH-35
Austin, TX 78744
RSVP FOR IN-PERSON OPTION RSVP FOR ZOOM OPTION
Background on the Search:
After 30 years of dedicated service, David Evans announced earlier this year he would be transitioning out of his role as Integral Care’s CEO. He remains in the position until his successor is in place. Integral Care’s Board of Trustees has been leading CEO succession planning efforts since the spring and regularly updating the public on its efforts through open meetings and announcements on its website here. Over the summer, this included sharing a survey with the community, collaborators, staff and stakeholders to gain insight into the qualities and strengths they are seeking in Integral Care’s new CEO.
After months of searching and interviewing highly qualified professionals, the Board has now narrowed its search down to three nationally acclaimed mental health leaders. After hearing from the public this week, the Board is slated to vote on a final candidate during its Board of Trustees meeting on December 14.
About Integral Care: Integral Care is committed to fostering health and well-being for individuals in Travis County, supporting those facing mental illness, substance use disorder and developmental disabilities. By providing essential services like a 24-hour helpline, ongoing counseling and housing assistance, we empower our community to regain independence. As the Local Mental Health and Intellectual and Developmental Disability Authority, Integral Care has pioneered high-quality, community-based care since 1967, collaborating with partners to build a supportive network and combat mental health stigma in Austin.
###
December 1, 2023
CEO Search – Meet the Candidates
Meet the Candidates
After a rigorous national search, Integral Care’s Board of Trustees CEO Search Committee has recommended three final candidates.
Please join us for our Meet the Final Candidates Forums. Each forum will provide an opportunity for attendees to learn more about the candidates and ask questions, as time allows. After each Q&A session, there will be an opportunity to personally meet the candidate.
Dates:
Candidate 1: Tuesday, December 5
Candidate 2: Wednesday, December 6
Candidate 3: Thursday, December 7
Time:
5:30 – 7:00 PM
Location:
Rudy Zapata Room, Integral Care’s Dove Springs
5015 S. IH-35, Austin, TX 78744
November 29, 2023
PES Hours
Effective Friday, December 1st, 2023, PES will resume normal business hours.
Monday-Friday: 8am-10pm
Saturday, Sunday: 10am-8pm
Holidays: 10am-8pm
November 20, 2023
Board of Trustees Meeting – November 27 2023
Meetings are open to the public.
Click here to watch the 11/27 Board of Trustees meeting live webinar.
Then, click the “Continue on this browser” button. The meeting starts at 5:30 pm.
November 14, 2023
Board of Trustees Meeting – November 2023
Meetings are open to the public.
Click here to watch the 11/17 Board of Trustees meeting live webinar. The meeting starts at 4:30 pm.
Click here to watch the 11/18 Board of Trustees meeting live webinar. The meeting starts at 9 am.
Then, click the “Continue on this browser” button.
October 24, 2023
Board of Trustees Meeting – October 2023
Meetings are open to the public.
Click here to watch the 10/26 Board of Trustees meeting live webinar.
Then, click the “Continue on this browser” button. The meeting starts at 5pm.
September 25, 2023
Board of Trustees Meeting – September 2023
Meetings are open to the public.
Click here to watch the 9/28 Board of Trustees meeting live webinar.
Then, click the “Continue on this browser” button. The meeting starts at 5pm.
September 14, 2023
Integral Care’s CEO Search
Integral Care is looking for its next CEO! Learn more about the role, who our ideal candidate is and more here.
August 21, 2023
Understanding the Impact of Extreme Heat on Mental Health
Wendy Amozurrutia-Salazar, Practice Manager, recently spoke to KUT about how extreme heat can impact not only our physical health, but also our mental health. Read or listen here.
July 14, 2023
St. John Clinic Ribbon-Cutting Ceremony
KUT, Spectrum News, CBS Austin, and KXAN recently ran pieces highlighting the ribbon cutting ceremony of the new St. John Clinic:
July 13, 2023
INTEGRAL CARE OPENS NEW CLINIC IN NORTH AUSTIN
Opening July 17, Integral Care’s St. John Clinic will offer integrated primary and mental health care for more than 5,000 adults and children in Travis County.
The clinic is located at 6937 N. IH 35, Austin, TX 78752. Lone Star Circle of Care will serve as the primary care provider, offering family medicine and pediatric services.
“Integrated primary and mental health care brings together health professionals such as psychiatrists, physicians, nurse practitioners, case managers under one roof. This team collaborates to support the whole person – body and mind – improving health outcomes for clients,” said Integral Care CEO David Evans.
Other services available at the location include counseling programs, wellness programs, a pharmacy for clients, and referrals to community resources. Administrative offices will also be onsite. In addition, the building will feature free meeting space for community members and murals painted by artists from Art from the Streets.
The St. John Clinic is located in an area of Travis County that is significant in Austin’s African American history. Beginning in 1869, the area hosted the annual Great St. John Encampment, dubbed “Black Austin’s homecoming.” African Americans from across Central Texas would make a pilgrimage to the St. John community for a social, religious, and educational conference.
Integral Care, along with collaborators Lone Star Circle of Care, Travis County and the City of Austin, will continue efforts to expand access to quality mental and primary health care that serves the diverse needs of our community.
“We only get the community that we deserve when we decide to build it together,” Travis County Commissioner Jeff Travillion said. “This is an opportunity to build something very special together.”
Over 100 people attended the ribbon cutting ceremony on July 12. Photos of the event can be downloaded here.
St. John Clinic Ribbon Cutting
From left to right: Integral Care Board of Trustees Member H. Ed Calahan; Integral Care Chief Equity Officer Dr. Amanda Banks; Integral Care Provider Network Authority Officer Louise Lynch; Lone Star Circle of Care Chief Financial Officer Brandon Teenier; Travis County Executive for Health and Human Services Pilar Sanchez; Integral Care Chief Executive Officer David Evans; Travis County Commissioner Jeff Travillion, Precinct 1; Integral Care Board of Trustees Chair Trish Young Brown; Integral Care Chief Operations Officer Dawn Handley; Integral Care Board of Trustees Member Emmitt Hayes; Dr. A.W. Anthony Mays of the St. John Baptist Association; Integral Care Chief Strategy Officer Anne Nagelkirk
For immediate mental health crisis support, call Integral Care 24/7 at 512-472-4357.
About Integral Care
Integral Care helps people build health and well-being so everyone has the foundation to reach their full potential. Integral Care supports adults and children living with mental illness, substance use disorder and intellectual and developmental disabilities in Travis County. Integral Care’s services include a 24-hour helpline for anyone who needs immediate support, ongoing counseling to improve mental health, drug and alcohol treatment to help with recovery, and housing to regain health and independence. Integral Care helps provide a strong foundation for well-being. Founded in 1967, Integral Care is the Local Mental Health and Intellectual and Developmental Disability Authority in Travis County. For more information, visit IntegralCare.org.
About Lone Star Circle of Care
Founded in 2001 in Georgetown, Lone Star Circle of Care (LSCC) is a Federally Qualified Health Center (FQHC) providing exceptional and accessible health care to nearly 100,000 patients in Bastrop, Bell, Burnet, Williamson, Travis, and Harris counties, most of whom are uninsured or underinsured. Throughout LSCC’s network of 27 clinic sites and a mobile unit, the health center provides the full spectrum of comprehensive primary care services, including Pediatrics, Family Medicine, Senior, OB/GYN, Mobile Mammography, Behavioral Health, Dental, Vision, and Pharmacy. Lone Star Circle of Care is committed to building healthy families and strong communities by connecting their patients with the services they need to achieve optimal health and wellness.
About Art From The Streets
The mission of Art From the Streets is to provide a safe and encouraging environment in which the positive spirit and creativity for those experiencing homelessness are nurtured through their own artistic expression. These artistic endeavors form a pathway to self-determination by means of the sense of achievement, social connections, and income generated through the pursuit of their art. Because focusing on housing alone does not achieve other equally important goals that are relevant and motivating to improving and sustaining a quality of life. For more information, visit artfromthestreets.org.
KUT, CBS Austin, and KVUE recently ran pieces highlighting the one-year anniversary of the 988 Suicide & Crisis Lifeline and Integral Care’s role in our community and the area our call center staff serve:
Check out this feature on Integral Care on the City of Austin’s YouTube channel.
The University of Texas at Austin’s Dell Medical School and LBJ School of Public Affairs have released a cost-saving analysis of The Inn, Integral Care’s 16-bed residential treatment program. The study found that The Inn saves taxpayers millions of dollars in public costs while improving outcomes for people experiencing a mental health crisis.
Mental Health Weekly talked to Integral Care about The Inn’s approach.
We are proud to receive national recognition from CrisisNow for our co-location at the 911 Call Center. Our collaboration with first responders streamlines the entire system of crisis care in our community. We have consulted approximately 30 other cities, states, and even a police department in Canada on our model. Our first responder friends, the City of Austin and Travis County are true collaborators helping move this innovation forward.
April 21, 2020
Kirk Watson: A True Champion for Brain Health
As our community grapples with COVID-19 and the impact on patients, healthcare workers and the healthcare system, we are beginning to recognize the toll this situation is taking on mental health. Whether it is an essential worker under pressure to perform on the job while worrying about exposure or someone with a compromised immune system isolated at home, COVID-19 is having short and long-term impact on our mental health. During these anxiety ridden times, it is reassuring to know that we have systems in place to address our community’s mental health needs and unexpected challenges.
The changes and concerns that have come with the COVID-19 pandemic are impacting the mental health and well-being of many in our community — with job losses, school closures, health concerns and separation from our loved ones. KXAN talked to Integral Care about how to support someone who may be experiencing a mental health crisis.
https://www.kxan.com/news/simplehealth/tips-on-identifying-and-responding-to-a-mental-health-crisis-during-covid-19/?fbclid=IwAR1R9AYe30k_x6zTVQTDj308qjMuFQFT2_xM0S5i4it4wFJYN7zGZcQcBvU
September 23, 2019
Integral Care Celebrates Completion of Terrace at Oak Springs

Integral Care marked completion of Terrace at Oak Springs with a Ribbon Cutting and Community Celebration. KXAN attended both events to learn more about this new 50-unit Housing First apartment community that supports recovery from homelessness, mental health issues and substance use disorder. Watch it here.
December 4, 2023
Integral Care Hosts Community Forums to Meet CEO Finalists
MEDIA ADVISORY
[For Immediate Release]
Media Contact:
Jessica Casarez
Jessica.Casarez@integralcare.org
Integral Care Hosts Community Forums to Meet CEO Finalists
AUSTIN, Texas (Dec. 4, 2023) – After a rigorous national search, Integral Care’s Board of Trustees CEO Search Committee has recommended final candidates. The Local Mental Health and Intellectual and Developmental Disabilities Authority is inviting members of the community to attend three open forums. Each event will feature an introduction to one of the candidates, followed by an opportunity for attendees to submit questions. After each Q&A session, the public will be invited to meet the candidates personally. Details of each forum are outlined below.
Dates:
Candidate 1: Tuesday, December 5
Candidate 2: Wednesday, December 6
Candidate 3: Thursday, December 7
Time:
5:30 – 7:00 p.m. CT
Location:
Rudy Zapata Room, Integral Care’s Dove Springs
5015 S. IH-35
Austin, TX 78744
RSVP FOR IN-PERSON OPTION RSVP FOR ZOOM OPTION
Background on the Search:
After 30 years of dedicated service, David Evans announced earlier this year he would be transitioning out of his role as Integral Care’s CEO. He remains in the position until his successor is in place. Integral Care’s Board of Trustees has been leading CEO succession planning efforts since the spring and regularly updating the public on its efforts through open meetings and announcements on its website here. Over the summer, this included sharing a survey with the community, collaborators, staff and stakeholders to gain insight into the qualities and strengths they are seeking in Integral Care’s new CEO.
After months of searching and interviewing highly qualified professionals, the Board has now narrowed its search down to three nationally acclaimed mental health leaders. After hearing from the public this week, the Board is slated to vote on a final candidate during its Board of Trustees meeting on December 14.
About Integral Care: Integral Care is committed to fostering health and well-being for individuals in Travis County, supporting those facing mental illness, substance use disorder and developmental disabilities. By providing essential services like a 24-hour helpline, ongoing counseling and housing assistance, we empower our community to regain independence. As the Local Mental Health and Intellectual and Developmental Disability Authority, Integral Care has pioneered high-quality, community-based care since 1967, collaborating with partners to build a supportive network and combat mental health stigma in Austin.
###
December 1, 2023
CEO Search – Meet the Candidates
Meet the Candidates
After a rigorous national search, Integral Care’s Board of Trustees CEO Search Committee has recommended three final candidates.
Please join us for our Meet the Final Candidates Forums. Each forum will provide an opportunity for attendees to learn more about the candidates and ask questions, as time allows. After each Q&A session, there will be an opportunity to personally meet the candidate.
Dates:
Candidate 1: Tuesday, December 5
Candidate 2: Wednesday, December 6
Candidate 3: Thursday, December 7
Time:
5:30 – 7:00 PM
Location:
Rudy Zapata Room, Integral Care’s Dove Springs
5015 S. IH-35, Austin, TX 78744
July 18, 2023
July 26 Virtual Community Forum
On Wednesday, July 26th at noon, Integral Care invites you to join us for a virtual Community Forum. In recognition of BIPOC (Black, Indigenous and People of Color) Mental Health Awareness Month, this virtual community forum will follow this year’s national theme, “Culture, Community, & Connection.”
Integral Care’s Chief Equity Officer and clinicians from across the agency will discuss:
• Cultural stigma associated with mental health
• Tips for finding culturally competent providers
• How healthcare experiences can be improved for BIPOC people
• Resources available for BIPOC communities.
https://integralcare.org/en/bipoc-mhm-2023/
May 2, 2023
May 24 Virtual Community Forum
The State of Children’s Mental Health

In recent years, we’ve seen significant increases in certain mental health disorders in children and youth, including depression, anxiety, and suicidal ideation. The COVID-19 pandemic era introduced a new set of challenges for children and youth in the U.S., but children and teens have been struggling for far longer. According to the CDC’s Youth Risk Behavior Surveillance System, feelings of persistent sadness, hopelessness, and suicidal thoughts and behaviors increased by about 40% among young people over the last 10 years leading up to the pandemic.
On Wednesday, May 24 at noon, Integral Care and NAMI Central Texas invite you to join us for a virtual Community Forum, “The State of Children’s Mental Health.” Clinicians and parents with lived experience will discuss the following topics:
- Factors that are negatively impacting children and youth the mental health
- Signs parents can watch for
- How to start the conversation around mental health
- Resources available for parents and caregivers
https://integralcare.org/en/cmh-forum/
March 9, 2023
March 30 Virtual Community Forum
Making a Difference: Peer Support in IDD Services
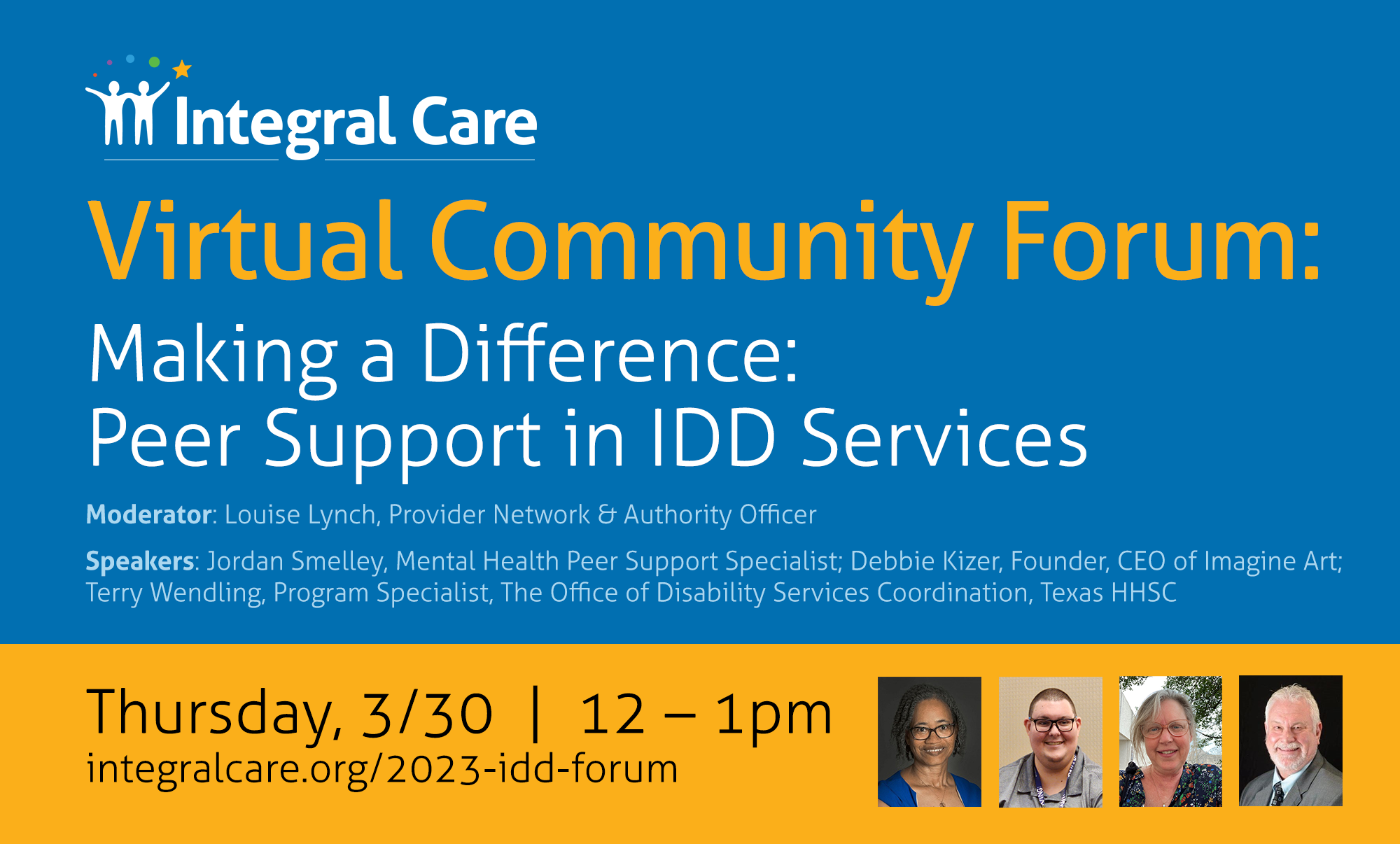
Individuals with an intellectual and / or developmental disabilities (ID/DD) suffer disproportionately with mental health conditions. Reasons often include stress related to frustrating social challenges and trauma such as physical, emotional, and sexual abuse, neglect and bullying. These inherent challenges create a unique susceptibility for the development of mental health conditions. Peer Support Services provide an opportunity for people with ID/IDD to develop social skills, learn how to advocate for their needs and give and receive mutual support from others with lived experience.
On Thursday, March 30 at noon, Integral Care invites you to join us for a virtual Community Forum, “Making a Difference: Peer Support in IDD Services.” Experts from across Texas will discuss the following topics.
- What Peer Support is and what Peer Support Specialists do
- How Peer Support Services for IDD came to be
- The current status of Peer Support in Texas, what’s on the horizon and how you can get involved
integralcare.org/2023-idd-forum
February 3, 2023
Central Texas African American Family Support Conference
To kick off Black History Month, a local event sheds light on mental health from the perspective of the African American community. Every February, Integral Care hosts the Central Texas African American Family Support Conference (CTAAFSC) to share mental health information and resources as well as build a community of support.
This year’s conference will take place Feb. 7-8 at the Palmer Events Center. The keynote speakers are Dr. Rheeda Walker, Professor of Psychology and Licensed Clinical Psychologist at the University of Houston, and Thabiti Boone, Former Obama White House Fatherhood Initiative Representative and New York Knicks Community Liaison.
Sessions will cover topics such as stigma around mental health in the African American community, health equity during the COVID-19 pandemic, and systemic barriers facing African American youth and their parents. Click here to view the schedule of events.
Established over 20 years ago, CTAAFSC was the first conference in Texas and only the third in the United States to focus on the healthcare needs of African Americans. The conference was born from a desire to confront the systems and cultural bias that have resulted in African Americans facing barriers to healthcare access.
November 19, 2022
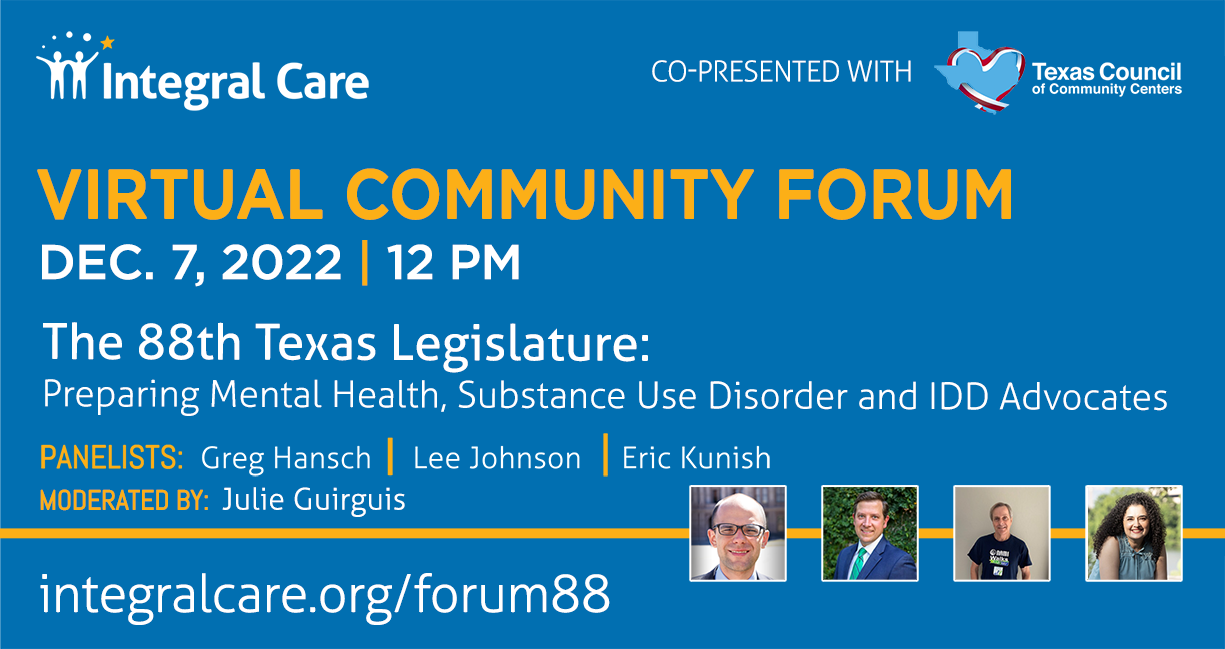
December 7 Virtual Community Forum
The 88th Texas Legislature: Preparing Mental Health, Substance Use Disorder and IDD Advocates
Over the last decade, the Texas Legislature has made an extraordinary commitment to mental health. Texas’ 88th Legislative Session kicks off on January 10, 2023. This creates more opportunities to further improve the issues affecting the mental health of Texans as well as the impact of substance use on our state and the needs of people living with intellectual and developmental disabilities (IDD).
On Wednesday, December 7 at noon, Integral Care and Texas Council of Community Centers invite you to join us for a virtual Community Forum, “The 88th Texas Legislature: Preparing Mental Health, Substance Use Disorder and IDD Advocates.”
October 21, 2022
Board of Trustees Meeting 10/27
The October Board of Trustees meeting will be held in person at 1430 Collier St, Austin, TX 78704, and will be streamed online.
Webinar link: click here
Join us every 3rd Wednesday of the month for this informative wellness series – the Together We Will Heal forum – that talks about mental health, substance use disorder, intellectual and developmental disabilities as well as the general wellbeing of African Americans. CTAAFSC’s vision is to educate the African American community on these topics and to provide resources around black mental health.
October 7, 2022
CTAAFSC Family Reunion
Renew, Empower and Advocate for Lasting Change
The Central Texas African American Family Support Conference (CTAAFSC) Committee is pleased to invite you to the CTAAFSC Reunion Day. Our theme is Renew, Empower and Advocate for Lasting Change (#REALChange).
Learn more & Register at https://ctaafsc.com/reunion/
September 15, 2023
Transparencies – September 2023
A Message From Our CEO:
September is an important time as we observe both National Recovery Month and Suicide Prevention Month. These observances call for action and provide opportunities to raise awareness around issues that impact us all.
Recent findings from the 2021 National Survey on Drug Use and Health, released by SAMHSA, underline the urgent need for our collective efforts:
- 46.3 million people aged 12 or older (or 16.5 percent of the population) met the criteria for having a substance use disorder in the past year, including 29.5 million people who were classified as having an alcohol use disorder and
- 24 million people who were classified as having a drug use disorder.
12.3 million adults aged 18 or older had serious thoughts of suicide in the past year, 3.5 million made suicide plans, and 1.7 million attempted suicide.
Integral Care is proud to be a cornerstone of support for our community.
August 3, 2023
Transparencies – August 2023
A Message From Our CEO:
The regular 88th Legislative Session ended in May, with two special sessions called by Governor Abbott to address remaining policy issues. In recent years, mental health has emerged as a critical public health issue, demanding urgent attention from policymakers and stakeholders alike. As economic challenges and events such as the COVID-19 pandemic continue to affect people’s well-being, the need for comprehensive mental health services and support has become increasingly evident. This session, Texas had an unprecedented surplus of $32.7B to work with and lawmakers negotiated a $321.3B budget. The Legislature appropriated $9.4B to behavioral health across 25 state agencies, a 15% increase from last session. Behavioral Health legislation was top of mind this session, with some notable behavioral health bills.
June 16, 2023
Integral Care’s CEO Succession Process
After 30 years of steadfast service, David Evans will be transitioning out of his role as Integral Care’s CEO by the end of 2023 – until his successor is in place. CEO succession planning efforts are led by Integral Care’s Board of Trustees and are underway.
Here, we will provide regular updates on important developments throughout the process.
June 2023
- The Board is reviewing proposals from executive search firms. Once a firm is hired, they will assist the Board in identifying qualified candidates for this position and our organization.
- We shared a survey with our community, collaborators, staff, and stakeholders to gain insight into the qualities and strengths they are seeking in Integral Care’s new CEO. The anonymous survey will close on July 17. You can take the survey here.
May 2023
- We announced that CEO David Evans is transitioning his role as Integral Care’s CEO to the next generation of leadership.
- We launched an RFP for executive search firms.
June 8, 2023
Transparencies – June 2023
A Message From Our CEO:
Last month, Integral Care, alongside Austin Public Health, the City of Austin, and Travis County, launched Ask, Listen, Talk, Repeat, a community-wide mental health awareness campaign designed to encourage conversations about mental health with our children and teens.
Each June, we celebrate Pride Month, a time to recognize the impact and contributions of LGBTQIA+ communities, and honor the 1969 Stonewall Uprising, a significant historical moment for the queer rights movement. This year, we also want to shine a light on LGBTQIA+ youth mental health.
May 1, 2023
Transparencies – May 2023
A Message From Our CEO:
May is Mental Health Month, a time to recognize the importance of taking care of our mental health. This Mental Health Month, we are excited to announce that Integral Care and NAMI Central Texas have partnered up again to create a Mental Health Month Toolkit. With growing concerns over the state of mental health among children and youth, the focus of this year’s toolkit is supporting the mental health and wellbeing of children and youth.
April 7, 2023
Transparencies – April 2023
A Message From Our CEO:
April is National Counseling Awareness Month, a time to raise awareness about the positive impact counseling can have on our mental health and well-being, and fight back against the stigma that still exists around seeking mental health care. It is also a time to recognize and honor the meaningful, and often life-changing, contributions counselors make each day.
Read more…
March 13, 2023
Transparencies – March 2023
A Message From Our CEO:
In celebration of Developmental Disabilities Awareness Month, I want to recognize the important work our team is doing in the community each day to ensure that adults and children with Intellectual and Developmental Disabilities (IDD) have the tools they need to build healthy relationships, live in the community and thrive.
Read more…
February 21, 2023
Transparencies – February 2023
A Message From Our CEO:
Each February, we celebrate Black History Month – a time to honor the legacy and achievements of Black Americans. At Integral Care, February also marks the annual Central Texas African American Family Support Conference – the first conference in Texas to focus on the healthcare needs of African Americans. Integral Care has sponsored this event for 23 years. This year’s conference, which took place last week, featured critical conversations around how adverse childhood experiences can impact adulthood, post incarceration syndrome, Black women, caregiving and parenting, and much, much more. People with lived experience shared inspiring stories. Professionals offered critical tools and resources. Meaningful relationships were built. I am grateful to the incredible conference Planning Committee for putting together another memorable and meaningful event that united and energized attendees and look forward to continuing the conversations that were started.
Read more…
January 24, 2023
Transparencies – January 2023
A Message From Our CEO:
Racism, discrimination, and inequity can significantly affect a person’s mental health. African Americans are 20% more likely to experience serious mental health issues than the general population and only one in three Black adults who need mental health care receive it. One study showed that 63% of Black people believe that a mental health condition is a sign of personal weakness. A lack of access to culturally competent care, mistrust in the American medical system, and a generational stigma related to recognizing mental health crises have created an environment where disparities in mental health care are far too common.
Every February, Integral Care hosts the Central Texas African American Family Support Conference (CTAAFSC) to share information and resources as well as build a community of support. Established over 20 years ago, CTAAFSC was the first conference in Texas and only the third in the United States to focus on the healthcare needs of African Americans. The conference was born from a desire to confront the systems and cultural bias that have resulted in African Americans facing barriers to healthcare access.
October 21, 2022
Transparencies – October 2022
A Message From Our CEO
Integral Care remains committed to eradicating institutional racism and structural inequities within our organization. At the recommendation of our Board/Staff Ad Hoc Committee on Racial Equity, Integral Care launched our interim Racial Equity Plan in May 2021. The interim plan was built from crucial conversations with our staff and collaboration with a national expert in the field of racial equity and cultural competency. It was also developed with the intent that racial equity would be incorporated into our strategic planning going forward. We updated our last Strategic Plan to include racial equity efforts and fully integrated it into the process of creating our new FY23-25 Strategic Plan.